What does good quality COPD care look like?
IPCRG is regularly asked by primary care clinicians to define good quality care. We take the view that primary care is person-centred, and therefore the best way to define quality is from the perspective of the person at risk of, or with the condition. From our regular conversations with expert patients and clinicians we have summarised what good quality care should look like from a patient perspective and how can clinicians provide that in 10 person-centred statements. These are divided into five areas: Prevention, Diagnosis and communication about the diagnosis, Management, Review and Referral. Our vision is that clinical teams will use them to benchmark their practice and potentially identify an area for improvement. Our own programme of work is steered by these statements. We are currently defining the competencies required to deliver them and the teaching methods and tools to enable delivery.
Leadership and capacity building
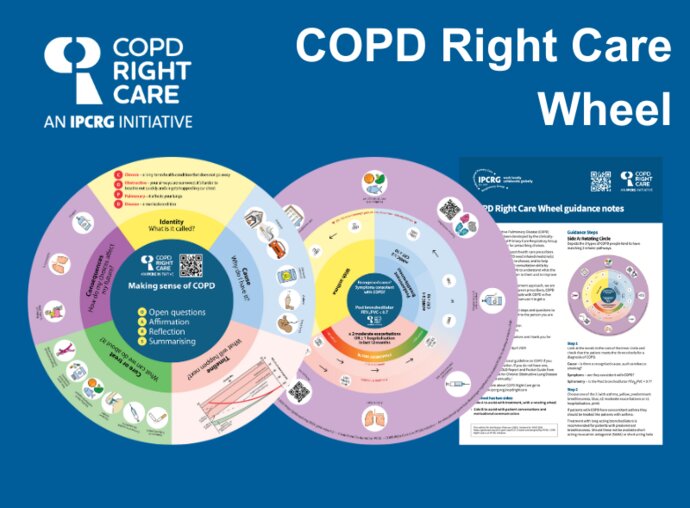
To achieve this quality of care, IPCRG advocates for two foundational programmes: developing leadership and capacity building. Primary care is cost-effective and the highest value input in a health system, delivering 90% of a person's health needs over their lifetime. Therefore, leadership is required to build respect for primary care and trust between different parts of the system. Capacity building of primary care teachers through education and training is also needed to underpin implementation, along with improvements to diagnosis so that interventions are allocated to the right people.
Therefore, IPCRG aims to extend its flagship Teach the Teacher programme to COPD and to work with our national COPD Right Care Delivery Teams to test innovative educational programmes (for example, by gamifying).
People with exposure to risk factors for COPD deserve...
1. Information, advice on mitigation and public health protection including local and personal risk factors.
People with COPD deserve...
Diagnosis and communication about the diagnosis
2. A primary care service that is competent and confident in diagnosing COPD including timely, accurate and objective tests, and information about COPD, its causes, the likely timeline, how it can be managed but not cured, and the consequences of decisions about treatment and self-management.
Management
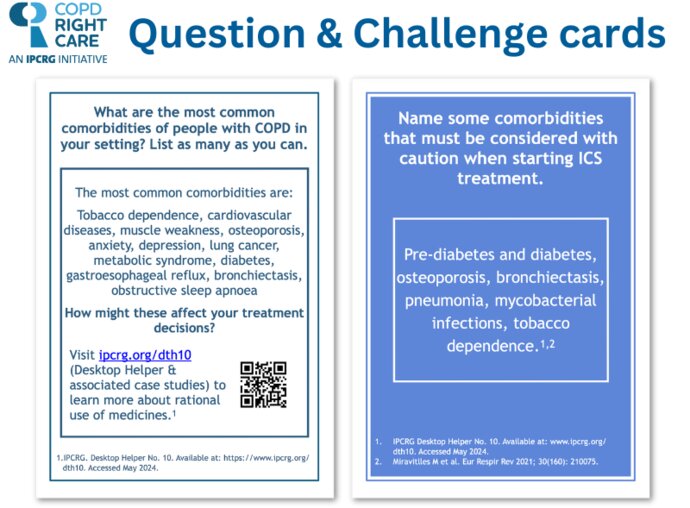
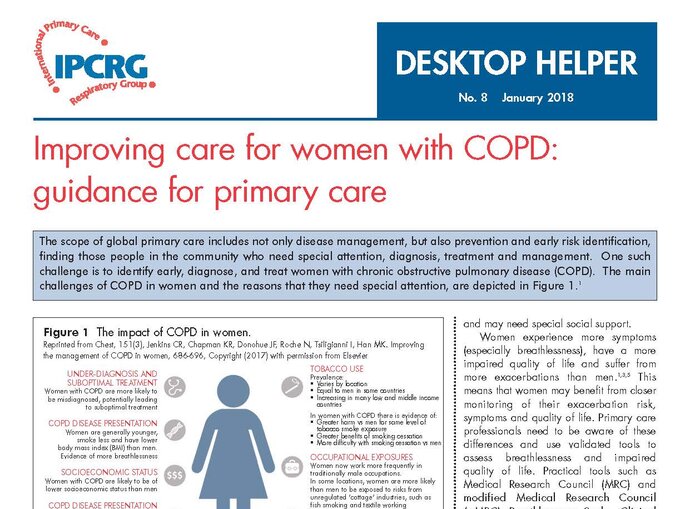
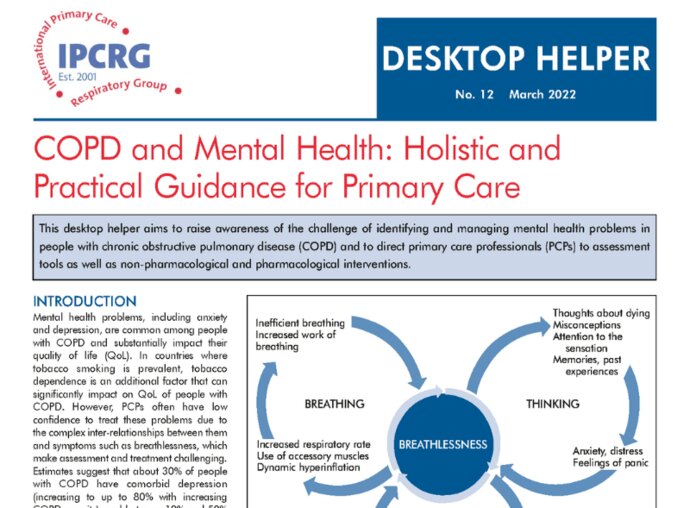
3. A primary care team competent to classify the stage and type of their disease over time using spirometry, quality of life and exacerbation history and competent to assess other morbidities.
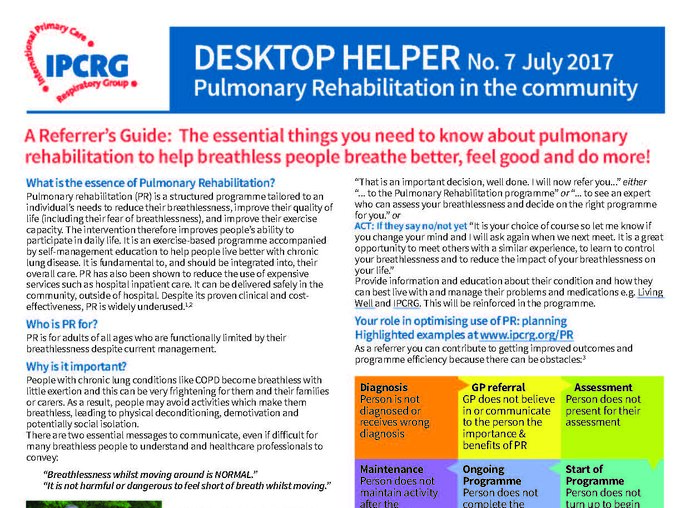
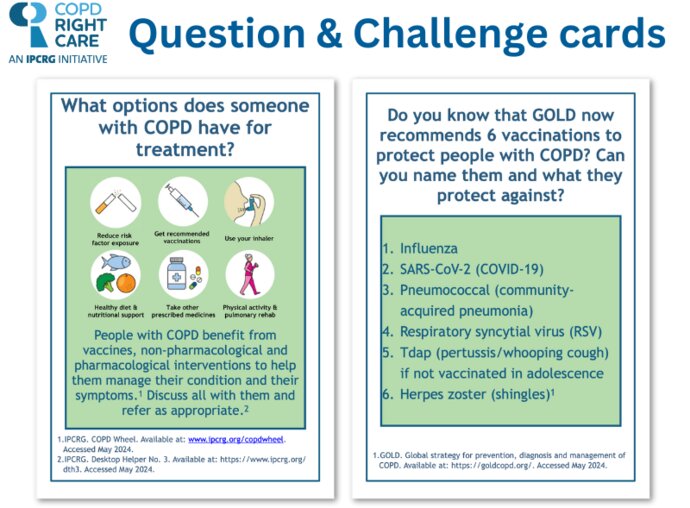
4. Long term holistic management according to the guidelines including vaccination, counselling and treatment if they are tobacco dependent, pharmacological and non-pharmacological treatment and referral eg to pulmonary rehabilitation, end of life care.
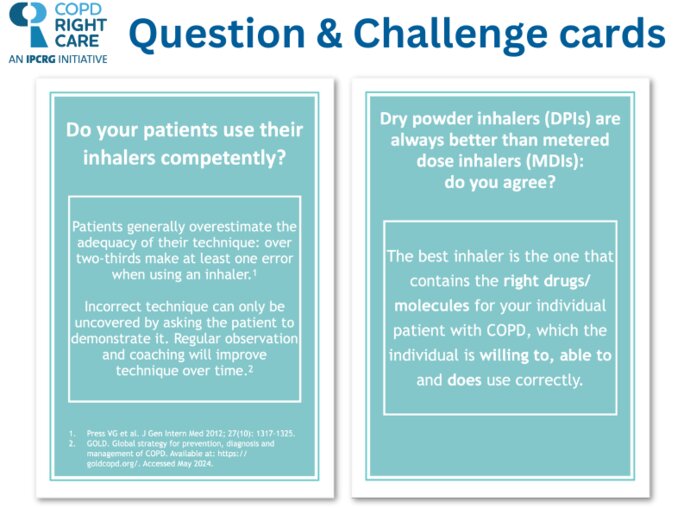
5. To be offered appropriate inhaler(s) according to their physical and cognitive abilities and characteristics and appropriate inhaler technique training by a primary care professional who knows the importance of eosophinil count and that bronchodilation is the basis of treatment.
6. Yearly flu vaccination, pneumococcal, Tdap, herpes zoster, RSV and COVID-19 vaccinations according to their history and national schedule.
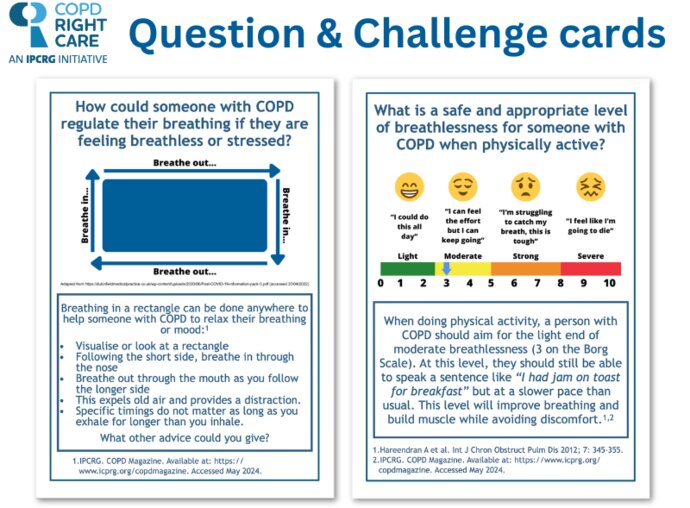
7. To agree an individualised self-management plan including recognition of exacerbations, smoking cessation, breathing exercises, nutrition, and physical activity taking into consideration mental and physical health, health literacy and access to care.
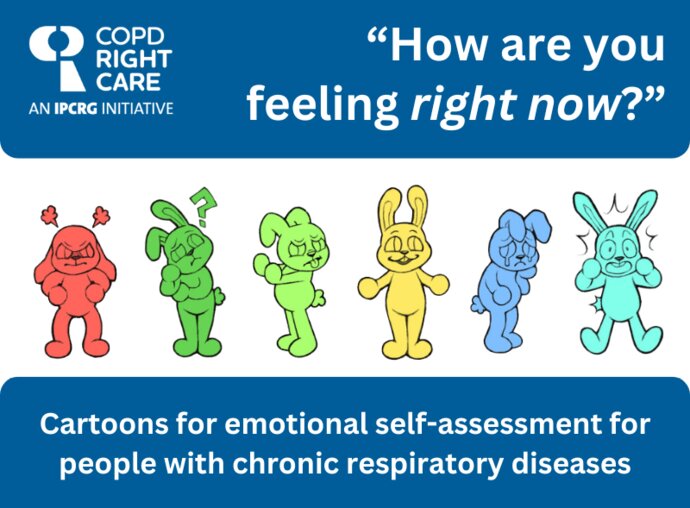
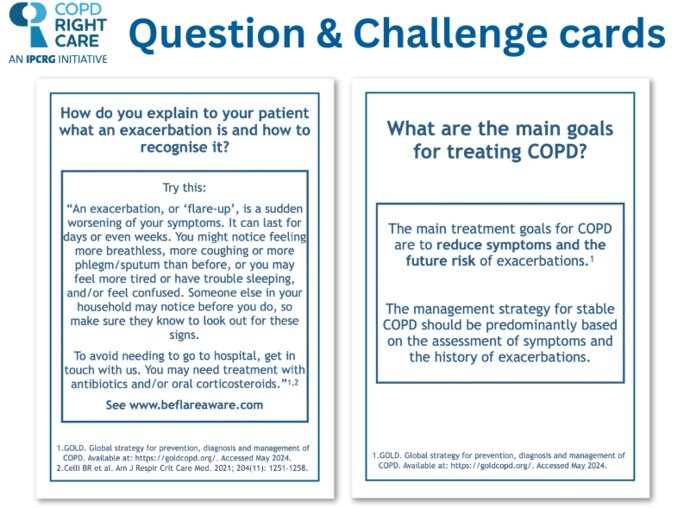
8. To be asked in a culturally appropriate way about exacerbations, to receive reassurance and appropriate treatment and to be followed up to ensure they have adequate support.
Review
9. A structured assessment of their symptoms, wellbeing, inhalation technique, future risk and support needs at acceptable intervals with additional follow-up after an exacerbation or a change in management.
When their COPD cannot be managed in their usual primary care
10. To have easy and timely access/referral to a primary or secondary health care professional who is skillful in COPD management whenever their COPD cannot be managed in their usual primary care.