Desktop Helper No. 3 - Improving the life of people with COPD by integrating a supportive and palliative approach from diagnosis to end of life - online version
This is an online version of Desktop Helper No. 3 - Improving the life of people with COPD by integrating a supportive and palliative approach from diagnosis to end of life. Visit the linked page for a PDF, translations, more information and related resources. References are available at the bottom of this page.
This desktop helper supports a long-term holistic approach to chronic obstructive pulmonary disease (COPD) management. The course and prognosis of COPD can be difficult to predict. Care is directed towards enhancing the quality of life of the individual and their family, slowing progression, reducing symptoms and preventing exacerbations, which is why palliative approaches are useful from the time the COPD diagnosis is communicated. It is important to remember that ‘palliative’ is a broad term for approaches that address individual needs across the spectrum of COPD.
Introduction
People live with COPD from years to decades, experiencing a lower quality of life (QoL), and greater functional limitations, anxiety and depression than others who are the same age without COPD. These potentially significant changes in QoL and expectations from life may be improved with enhanced care, highlighting the need for a long-term and holistic approach to support people with COPD, their family and caregivers. Care selection is based on repeated discussion during the evolving prognosis and symptom trajectory, identifying and minimising distressing symptoms and ensuring medical, physical, social and spiritual support. This may include supporting access to supportive and financial care packages from social care and other non-medical services. (1) From beginning to end, COPD must be treated using all available appropriate therapies for COPD AND the common co-morbidities such as cardiovascular disease (CVD), depression/ anxiety, diabetes, renal disease, lung cancer and osteoporosis. Treatment must be based on appropriate evaluations and knowledge of the person’s functional status and personal goals at each stage of COPD stabilisation and progression (e.g. evaluated at least annually). Variations will depend on the local availability of healthcare and therapies, cultural norms and the individual’s beliefs and goals.
Impact of COPD
COPD is a chronic disease that impacts every aspect of life and is often diagnosed after months or years of people reducing or eliminating activities to lessen breathlessness or feelings of “air hunger” or fatigue. For people living with COPD, breathlessness may be due to a combination of factors including common comorbidities such as heart disease or anxiety. (2,3) COPD lowers overall QoL including social interactions, mood, work, family life and self-care (Figure 1). (4)
Including the preferences of the person with COPD in their long-term care
A crucial step in the longitudinal care that primary care can provide is understanding the individual’s current state by assessing symptom burden (perhaps using the COPD Assessment Test available at https://www.catestonline.org/), functional abilities (e.g. ability to do what they consider important – work, family and social interactions, self-care), the frequency and severity of exacerbations (e.g. may be labelled as episodes of “bad colds” or “acute bronchitis”), and ideas, concerns and expectations (ICE) such as losing independence, ability for self-care or having to live in a “nursing care facility”). The individual with COPD and their family may share feelings, frustrations and concerns about future needs with others in our primary care teams and we can also use this information and these team members, help to open important discussions. People living with COPD remind us — “If you ask us questions then LISTEN to our answers” (Table 1).
Table 1: The perspectives of people with COPD—what my healthcare team needs to know!
- My healthcare team needs to know who I am and what my functional status is and what my goals are. Without this baseline, many of the conservations take too long or are meaningless.
- Ask me “What is a usual day’s activity like for you? What have you had to give up or modify over the last few years? What do you not want? e.g. I never want to go to a nursing home.”
- Ask me “What are your thoughts about your life over the next year or if your COPD gets worse?” This is probably best done during in-person visits where the clinician can read body language and give more support.
- Ask me “What do you and your family want us to know and put in your medical record about your goals and future plans?”
- Many of us don’t know what we don’t know or what to ask. Let us know what our options are by sharing information, a website link or someone to talk to.
- Finally, if you ask then LISTEN to our answers.
___________________
Thanks to the people with COPD who allowed Barbara Yawn to interview them.
Table 2: Questions to ask to guide broader care and to record in the medical record
Table 2 provides questions to guide discussion on long-term care to help you explore the broader aspects of care and identify those areas of greatest importance to each individual.
Table 2: Questions to ask to guide broader care and to record in the medical record
Essential questions to be asked at each visit:
- What brings you here/to this visit?
- Any special concerns from you, your family or your carer?
Questions to be asked over subsequent visits to help to develop an understanding of
personalised needs and goals to direct support:
- What is your understanding of where you are with your COPD at this time?
- What are your fears and worries for the future?
- What are your goals……if time is short?
- What outcomes/consequences/results would be unacceptable to you?
___________________
See our online Supplementary material S1 for additional questions to help with your conversations with individuals and their families. Listen to author and surgeon Atul Gawande discuss the importance of these four questions to understand people’s priorities at https://www.bbc.co.uk/programmes/b04tjdlj
An important advantage of care continued over months and years is that the conversations are built upon our previous discussions – our knowledge is cumulative and evolving. Understanding and document-ing what the individual and family wants regarding goals, future plans and end of life care/living wills, can ensure their preferences are recorded and available when care may include hospital specialists or hospitalisation. These questions can be set in the Open questions, Affirmation, Reflective listening, Summarising (OARS) framework (see the IPCRG Desktop Helper COPD and mental health www.ipcrg.org/dth12) that helps establish and maintain rapport, assess the individual’s needs and personalise your counselling and education responses. (5)
Learning about community resources
To make plans, people need to know what is available to them. Information on local and regional resources needs to be gathered and shared with them, most usefully by someone in the primary care team. In addition, home visits and telehealth video visits may show you where and how the person with COPD lives to facilitate better understanding of opportunities to support their interests and needs for living with COPD and any associated comorbidities.
See how Seneth Samaranayake, a GP in Sri Lanka, takes a palliative approach using the resources available in his community in our Supplementary material S2.
Actively managing symptoms including breathlessness
People with COPD may have many symptoms including fatigue, breathlessness, cough, depression, anxiety and sleep disturbance that each require relieving (“palliative”) treatment. These can be offered by every primary care clinician working holistically and attending to each and all of the person’s needs, irrespective of life expectancy.
Non-drug treatments
Evidence-based smoking cessation is the most effective intervention to slow the progression of COPD in people who are tobacco dependent (see the IPCRG Desktop Helper Helping patients quit tobacco) (6) and employ the Ask, Advise, Act approach at every consultation. (7) Quitting success will be improved if tobacco dependence medicines and support services like “quit lines” are also used. (6)
Pulmonary rehabilitation (PR) is effective in reducing breathlessness and fatigue and improving health status and exercise tolerance and can reduce rehospitalisation in those who have had a recent exacerbation. It also can reduce symptoms of anxiety and depression. (8,9) Read more at: www.ipcrg.org/PR.
Breathlessness is the most common symptom in people with COPD and can be challenging to manage. The severity of breathlessness may bear little relationship to the severity of COPD as measured by lung function, with more than 40% of people with mild COPD experiencing moderate to severe breathlessness. (10( However, there are a number of non-pharmacological interventions in addition to PR that may also be suggested depending on the cause and individual preferences. (11-13) A range of possible interventions are shown in Table 3.
We have insufficient data to present evidence levels to support widespread use of other interventions for breathlessness such as positive psychology, singing therapy, self-hypnosis and laughter therapy, but they may be useful, balancing individual preferences and risk assessment. When available and feasible to use, non-invasive ventilation may also reduce daytime breathlessness in people with advanced breathlessness. (8)
Table 3: Non-pharmacological interventions to address breathlessness and exercise capacity
- Pulmonary rehabilitation - Can relieve breathlessness and fatigue, improves emotional state and enhances person’s sense of control over their condition – moderately large and clinically significant improvements.
- Facial cooling with a fan or cool flannel. See this video - Good evidence of short-term benefit from using a fan (static or hand held), relieving breathlessness at rest and reducing recovery time after activity. Movement of air over a person’s face is thought to stimulate a vagal response. A cool flannel is an alternative.
- Mindfulness/meditation - 20-minute mindful breathing reduces breathlessness in lung disease, and anxiety/depression in advanced disease; enhances non-evaluative attention and may increase self-efficacy
- Relaxation techniques - Some evidence can help anxiety, breathlessness and fatigue in COPD. Guided imagery (‘thinking of a nice place’), progressive muscular relaxation and counting are most acceptable
- Pacing - May help breathlessness as a component of an evidence-based complex intervention
- Walking aids - Can improve exercise capacity
- Cognitive behavioural therapy - Problem-solving approach that challenges unhelpful thoughts/ behaviours; reduces anxiety in COPD in short term; increases pulmonary rehabilitation attendance.
- Breathing techniques - Most studies do not find this intervention improves breathlessness, although some evidence in lung cancer and pursed lip breathing may help in COPD; however, these are a key component of evidence-based complex interventions for breathlessness
- Acupuncture/pressure - Improves breathlessness in advanced disease and may reduce anxiety
- Inspiratory muscle training - Conflicting evidence for impact on breathlessness; people need to be carefully selected
_______________
See our Supplementary material for a full list of supporting references
Drug treatments to be used together with non-pharmacological interventions
Inhaled bronchodilators are the first line COPD pharmacotherapy. (8,13) Whenever possible, use long-acting single or dual bronchodilators which can improve breathlessness, and reduce hyperinflation thereby reducing symptoms and in some people also reducing the risk of future exacerbations.(13) Add corticosteroids when frequent exacerbations cannot be prevented with bronchodilators, by trigger avoidance or, if available, PR. (8) Neither inhaled or oral corticosteroids are considered therapy for breathlessness.8 Additional drug options targeted at relief of breathlessness should be considered only after other options have been exhausted. (12)
Morphine Regular, low dose, oral sustained-release morphine is effective in relieving chronic disabling breathlessness and should be titrated to effect and reviewed regularly. (14,15) Regular use of morphine may require management of constipation, nausea and vomiting, particularly in the first week of administration. For those people with very advanced, often called end-stage, COPD who are appropriate for hospice or end of life care, low-dose, immediate-release morphine can extend exertional endurance time. (8,16-18)
Benzodiazepines are used in some countries for the relief of breathlessness. However, a recent Cochrane review found no evidence either for or against the use of benzodiazepines in this way. (19) Use should be based on balancing risk and potential benefits and may vary by what other resources are locally available.
Oxygen therapy There is evidence that people with COPD who are hypoxic at rest (e.g. at rest SpO2 <92%) may benefit from long term oxygen used 10 to 15 hours daily. Oxygen has not been shown to improve mortality or morbidity for people who are breathless but not hypoxic. Oxygen should not be routinely prescribed for people with stable COPD or resting- or exercise-induced moderate desaturation. (8) Yet there is substantial variation globally of oxygen prescribing in primary and secondary care. Latest reviews suggest that the risks of oxygen for people who are not hypoxic outweigh the benefit and suggest it is the movement of air over a person’s face which stimulates a vagal response rather than the oxygen that is helpful. (12) Whilst individual factors must be considered, it is also important to explain the risks and benefits of supplemental oxygen use to people with COPD and caregivers because they often overestimate the benefits and underestimate the risks. During the COVID-19 pandemic, oxygen has become a scarce resource and therefore we need to align its use with the evidence wherever possible. Use pulse oximetry or blood gases to determine oxygen saturation and need for supplemental oxygen. (8) Rather than prescribing oxygen, try prescribing a handheld fan blowing air onto the face (this may stimulate a vagal response) or applying a cool flannel to the face (See: https://www.youtube.com/watch?v= y5tBC5R8DYs). (20)
This like many areas of clinical practice requires local interpretation. Clinicians need to know the evidence as well as have an awareness of local practice and beliefs which may vary from the evidence led by tradition, “specialist practice” or local systems. Awareness of the evidence allows clinicians to provide people with COPD and their carers with more informed choices to support best use of limited resource.
Managing malnutrition
Fatigue, muscle weakness and overall health status can all be improved with nutritional support. (8) About 1 in 5 people with COPD are at risk of malnutrition, particularly under nutrition, causing poor outcomes and increased healthcare costs due to loss of skeletal muscle (sarcopenia) and lean tissue mass (cachexia). Malnutrition can result from inadequate local access to food or from inability to shop and cook among other reasons. Calculate body mass index (BMI) and track weight loss in the office or by the person at home. When available, a simple measure like handgrip strength can be used as a marker of muscle strength. If malnutrition is a concern, it is necessary to explore reasons for the malnutrition and try to identify solutions which may include better food access, setting goals to increase body weight and muscle mass, exploring eating habits and identifying food support systems. A useful pathway for guidance on managing malnutrition in COPD is available at www.malnutritionpathway.co.uk/copd/. Quitting smoking may help to improve appetite and taste.
Role of Primary Care Team
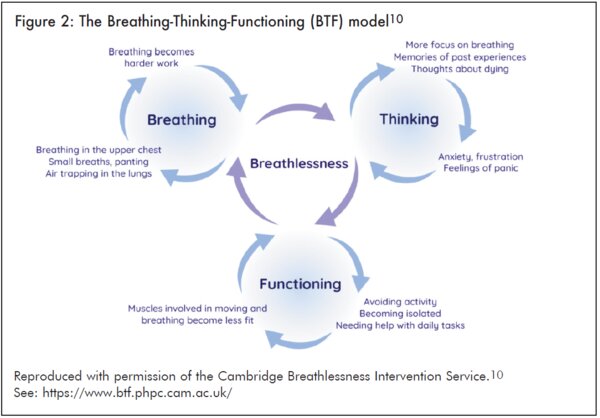
People with COPD attend primary care throughout their life, and therefore primary care must respond to their changing need for symptom relief which is independent of disease severity. Responding to people’s changing needs may include being mindful of alternative communication methods including the telephone or tele-video that enables regular contact with no travel effort. (1) A model that can work in high and low income settings (See our online Supplementary material S2) is the allocation of a health care professional or “coach” with specific COPD knowledge to support the individual over the course of their life and as their needs change and guide them to locally available health and social services, faith organisations and online self-help resources. Tools such as questions in Table 1 can guide the discussion. Consider establishing a register of people for whom discussions around advance care planning would be appropriate. Such discussions should then be recorded and dated and revisited at regular intervals. The Breathing Thinking Functioning model (10) has been found by primary care clinicians in the UK to be a very helpful and practical way to think about and manage disabling breathlessness by breaking three linked vicious cycles using a range of low-cost non-drug interventions that are easily taught, e.g. lengthening the out-breath, compassionately challenging misconceptions such as expecting to die gasping for breath, explaining that becoming moderately breathless by being active is not harmful and will actually build fitness in muscles and will lead to improved breathing (Figure 2).
Primary care can coordinate care locally from health care and other community organisations that is tailored to the individual’s needs. We can discuss concerns about dying and preferences for future management.
Role of Carers and Family
Most people with COPD only interact with the health system for a few hours or days a year. Therefore recruitment of support from carers, family and community members will be essential to supplement what primary care can offer. Primary care has a role to offer education directly or through trusted third parties to these informal carers about:
- Correct use of inhalers (e.g. COPD Foundation, AsthmaLungUK)
- Breathing positions e.g. sitting upright or leaning forward, standing leaning against a wall or forward against a chair or lying on your side with head propped up with pillows
- Breathing techniques such as pursed lip breathing or diaphragmatic breathing
- Energy conservation by planning ahead, sitting during tasks, minimising arm movements, avoiding boom-bust cycles of doing too much when you feel well, nutrition, and use of inhalers. Helpful leaflets can be found at: https://www.acprc.org.uk/publications/ patient-information-leaflets/
- Nutrition
- Meditation
Advance care planning and end-of-life care
People with COPD and their families need the support of trained clinicians to discuss advance care plans including end of life care: non-invasive ventilation, preferred place of death, Do Not Resuscitate decisions/orders and the use of advance directives or living wills. (21) Those plans must be clearly recorded since people with COPD tend to die from CVD, heart failure or lung cancer and their care may be shared or transferred to other groups of health care professionals. Plans and preferences should not be static and must be reviewed and updated regularly as their and their family’s circumstances evolve. For example, it is important to review using questions such as “Before, you thought you would like… Is that still what you would like?” Asking about death and dying can be intimidating and uncomfortable for many HCPs but people with COPD and their families appreciate the opportunity for these discussions (See our online Supplementary material S3).
COPD can have multiple trajectories (Figure 3) from progressive and often unrecognised disabling breathlessness, pain, anxiety and depression to sudden events and death during acute exacerbations or cardiac events against a background of long-term decline. Even where hospices are available, they may not meet the needs in all these events. Some events can help highlight the need to discuss palliative and end of life care. Half of people admitted for COPD and acute respiratory failure will typically die in the next two years. This could be a key indicator for inclusion in the palliative care register and updating or completing a living will, if these are available. The palliative care approach requires repeated assessments of current status, available resources, involving the person and family desires and capabilities, bringing whole systems and available services together to meet the full range of needs. Since it is often not possible to predict the trajectory for individual people, especially as they near end of life, having discussions earlier to supplement discussion during an event is important. Be clear that predicting trajectories and ‘time left’ is difficult and often uncertain but reassure the person that support is available and their wishes will be respected. Include family and carers to ensure that the person’s wishes are known and feasible to accomplish.
Dying
The aim is for people with COPD to die in their preferred place. This may be at home. However, this preference may change over time as a person experiences changes in their condition and realises what supports are not able to be provided at home. For example, their preference may change to a hospice. For this reason, advance planning should be viewed as a dynamic process involving sensitive discussions with the individual and their families that should be revisited over time and records updated accordingly. See our Supplementary material S5 for examples of formularies for end-of-life prescribing.
Additional Information
Authors: Barbara Yawn, Matteo Mannucci, Seneth Samaranayake and Siân Williams
Contributor: Anna Spathis
Reviewers: Nicholas Glasgow, Steve Holmes, Katherine Irene Pettus
Editor: Tracey Lonergan
This desktop helper was self-funded by the IPCRG.
This desktop helper is advisory; it is intended for general use and should not be regarded as applicable to a specific case.
Creative Commons Licence Attribution-NonCommercial-NoDerivatives.
The IPCRG is a Scottish-registered charity (No. 035056) and a Scottish company limited by guarantee (Company No. SC256268). Communication address: 19 Armour Mews, Larbert, FK5 4FF, Scotland, United Kingdom.
Resource information
- COPD
- End of Life
- COPD Right Care
- COPD
- Management
- Clinical Education