What is the variation in symptoms for different variants of SARS-CoV-2, why do we see this variation and are there predictors for acute disease severity?
What the research says:
The main symptoms of early variants of SARS-CoV-2 were a high temperature, a persistent cough and a loss of smell or altered sense of smell. Over 20 symptoms are now acknowledged as part of the constellation of symptoms of SARS-CoV-2, some of which are common across variants and other which are more likely to be associated with one variant over another.
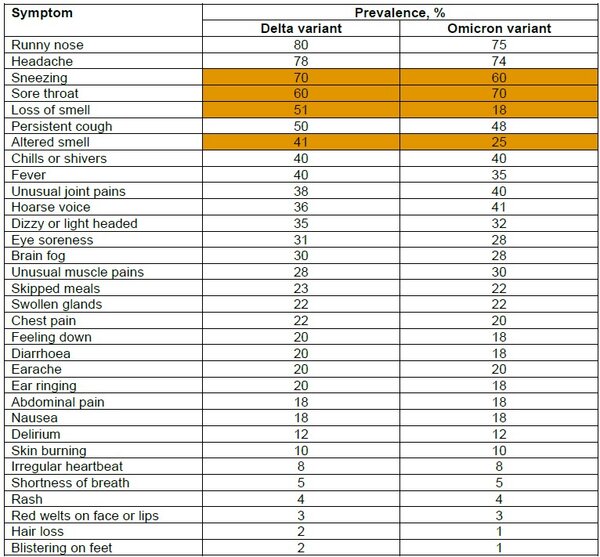
Variation in symptoms by SARS-CoV-2 variants (adapted from Menni et al 2022)
Values estimated from graphical presentation. Orange indicates symptoms occurring at least 10% more frequently with either variant vs the other.
The reasons for the variation in symptoms profiles in under investigation. There is some suggestion that the Omicron variant is less effective in infecting the cells of lower respiratory tract and so less likely to cause the more severe pneumonia, lung damage and systemic organ damage associated with other variants (Menni et al 2022).
The strongest predictors for a severe COVID-19 disease course include an immunosuppressed state, older age (graded increase in risk with advancing age), multiple pre-existing comorbidities, hypoxia, extensive lung involvement (on imaging), multiple laboratory abnormalities and biomarkers of organ dysfunction (Gallo Main et al 2021). Symptom-based predictors of the likely severity of COVID-19 illness have proved less useful than risk assessment based on patient characteristics (e.g. immune status) and the presence of comorbid conditions. There is some suggestion that patients presenting with multiple symptoms assessed as severe may be more likely to progress to requiring hospitalization (Sudre et al 2021).
What this means for your clinical practice:
- Compared to the Delta variant, the Omicron variant is associated with an increased prevalence of sore throat and a lower prevalence of loss or altered smell and sneezing.
- Individual patient risks should be considered rather than symptoms, although the number of symptoms may be a predictor for hospitalisation. Continue to base risk on individual patient risk characteristics, not severity of symptoms on diagnosis. Conduct a broad assessment that includes pulse oximetry in patient follow up.
With grateful thanks to Tiago Maricoto, MD, PhD (Family Doctor, Aradas Health Unit and University of Beira Interior, CACB-Clinical Academic Centre of Beiras, Portugal) for and on behalf of the IPCRG practice driven answers review group.
Useful links and supporting references:
Gallo Marin B, et al. Predictors of COVID-19 severity: A literature review. Rev Med Virol 2021;31:1–10. Available at: https://pubmed.ncbi.nlm.nih.gov/32845042/. Accessed May 2022.
Menni C, et al. Symptom prevalence, duration, and risk of hospital admission in individuals infected with SARS-CoV-2 during period of omicron and delta variant dominance: a prospective observational study from the ZOE COVID Study. Lancet 2022;399:1618–24. Available at: https://www.thelancet.com/action/showPdf?pii=S0140-6736%2822%2900327-0/ Accessed May 2022.
Sudre C, et al. Symptom clusters in COVID-19 : a potential clinical prediction tool from the COVID Symptom Study app. MedRxic 2020.06.12.20120956. Sci Adv 2021;7:eabd4177. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7978420/. Accessed May 2022.
Resource information
- COVID-19
- Diagnosis
- Disease management