How should post COVID tiredness and fatigue be managed?
What the research says:
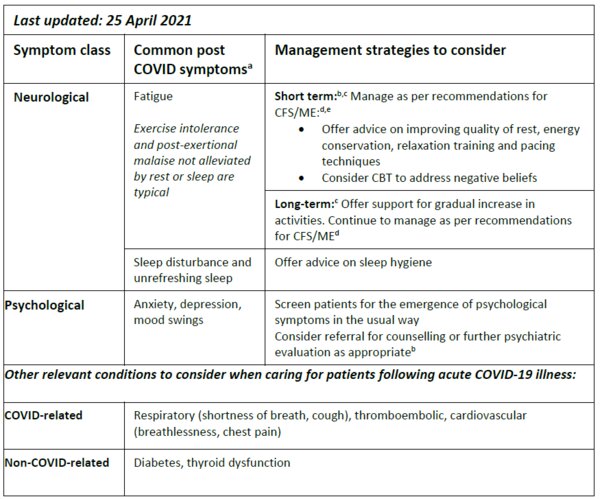
Following an acute COVID-19 illness patients report a variety of persistent symptoms including pulmonary (shortness of breath, cough), neurological (fatigue, headache, difficulty concentrating, memory loss, sleep disturbance, loss of smell, paraesthesia), psychological (anxiety, depression, mood swings), cardiovascular (breathlessness, chest pain), musculoskeletal (non-specific pain, myalgia) and low grade fevers. Here we focus on the management of tiredness and fatigue (NHS 2021).
Tiredness and fatigue are the most commonly reported long-term symptoms following SARS-CoV-2 infection, including among those with mild COVID-19 illness (Kashif et al 2021). There are currently no data to indicate whether these symptoms are more common following COVID-19 illness compared with other viral illnesses. Symptoms of tiredness and fatigue may persist for
weeks/months after recovery from acute illness (Townsend et al 2021) and for some patients they may form part of a constellation of persistent symptoms referred to as long-COVID or post-COVID syndrome (Nalbandian et al 2021). There are currently no specific guidelines on the optimal management of persistent tiredness and fatigue among patients following COVID-19 illness. Potential parallels with chronic fatigue syndrome/myalgic encephalitis (CFS/ME) suggest that management of post-COVID-tiredness/fatigue should be managed as for these conditions with energy conservation and gradual increase activities (Gaber 2021; Greenhalgh et al 2020).
What this means for your clinical practice:
- Continue to use appropriate personal protective equipment and infection control measures when seeing patients following acute COVID-19 illness
- Reassure patients that for most people symptoms will resolve over weeks/months
- Focus on symptom relief and careful monitoring for the emergence of serious sequalae.
- Manage tiredness and fatigue as per recommendations for CFS/ME (CDC 2021)
- Manage physical pain and recurrent headaches with simple analgesia (paracetamol [also known as acetaminophen] or ibuprofen).
- Consider common neurological and psychological issues as potential contributors to tiredness or fatigue and screen for and manage as appropriate.
- Consider appropriate referrals when fatigue is persistent, worsening, or not responsive to non-pharmacological intervention
CBT, cognitive behavioural therapy ; CFS/ME, chronic fatigue syndrome/myalgic encephalitis.
aNational COVID-19 Clinical Evidence Taskforce. Caring for people with COVID-19. Available at:
https://covid19evidence.net.au/. Accessed April 2021
bGreenhalgh T, et al. BMJ 2020;370:m3026. Available at: https://www.bmj.com/content/bmj/370/bmj.m3026.full.pdf. Accessed April 2021.
cGaber et al. Prog Neurol Psych 2021 ;25 :36-9. Available at : https://wchh.onlinelibrary.wiley.com/doi/10.1002/pnp.698. Accessed April 2021.
dCDC. Myalgic encephalomyelisits/chronic fatigue syndrome. Available at: https://www.cdc.gov/me-cfs/treatment/index.html. Accessed April 2021.
eThe ME Association. Management. Available at: https://meassociation.org.uk/about-what-is-mecfs/management/. Accessed April 2021.
Resource information
- COVID-19
- Long COVID
- Disease management