After serious pathology has been excluded, how do we manage common post-COVID symptoms?
What the research says:
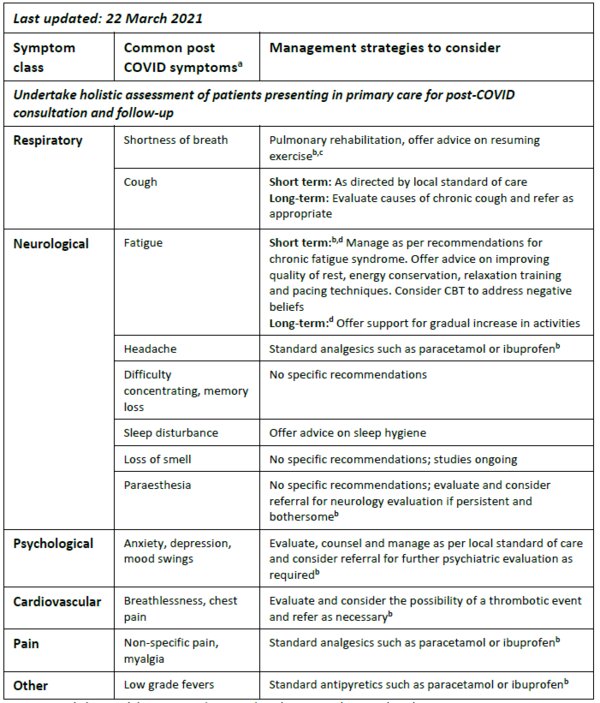
For some patients, post-COVID symptoms may persist for weeks/months after recovery from acute illness. Common symptoms include pulmonary (shortness of breath, cough), neurological (fatigue, headache, difficulty concentrating, memory loss, sleep disturbance, loss of smell, paraesthesia), psychological (anxiety, depression, mood swings), cardiovascular (breathlessness, chest pain), musculoskeletal (non-specific pain, myalgia) and low grade fevers. There are currently no specific guidelines on the optimal management of persistent symptoms and clinical sequalae among patients following COVID-19 illness. Anosmia is emerging as a common and troublesome persistent symptom and studies are ongoing to evaluate potential management strategies. The WHO recommends tailored, individualised management including pulmonary rehabilitation where appropriate.
What this means for your clinical practice:
- Before considering onward referral, conduct a holistic assessment of patients presenting in primary care with persistent symptoms following an acute COVID-19 illness including assessment of mental health and other non-COVID issues and manage these as appropriate
- Management of patients with persistent post-COVID symptoms should focus on symptom relief and careful monitoring for the emergence of serious sequalae such as pulmonary embolism (or other thrombotic complications) and pulmonary fibrosis.
- Reassure patients that for most people symptoms will resolve over weeks/months. Educate patients to be aware of and report new symptoms and to act promptly to seek medical attention for chest pain.
- Pulmonary rehabilitation may be beneficial for patients with persistent shortness of breath or deconditioning. Offer advice on the importance of resuming exercise.
- Assess patients for the emergence of clinical depression or anxiety and manage according to local guidance.
- Evaluate and consider appropriate referrals for respiratory, psychiatric, cardiovascular or neurological symptoms.
CBT, cognitive behavioural therapy; DVT, deep vein thrombosis; PE, pulmonary thrombosis. aNational COVID-19 Clinical Evidence Taskforce. Caring for people with COVID-19. Available at: https://covid19evidence.net.au/. Accessed March 2021 bGreenhalgh T, et al. BMJ 2020;370:m3026. Available at: https://www.bmj.com/content/bmj/370/bmj.m3026.full.pdf. Accessed March 2021. cWHO. COVID-19. Clinical Management. Living Guidance, 25 January 2021. Available at: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-1. Accessed March 2021 dGaber et al. Prog Neurol Psych 2021 ;25 :36-9. Available at : https://wchh.onlinelibrary.wiley.com/doi/10.1002/pnp.698. Accessed March 2021.
Resource information
- COVID-19
- Long COVID
- Disease management