Desktop Helper No.14 - Quick guide to spirometry - online version
This is an online version of Desktop Helper No.14 - Quick guide to spirometry. Visit the linked page for a PDF, translations, more information and related resources. References are available at the bottom of the page.
This desktop helper aims to provide primary care professionals with the information they need to prepare for, conduct, evaluate and interpret spirometry and understand its role and limitations in the diagnosis and monitoring of respiratory disease.
Introduction
Spirometry is an objective test that measures the volume of air a person can exhale and the speed (flow) at which they can do so.(1-6) It is mandatory in diagnosing and monitoring chronic obstructive pulmonary disease (COPD), and important for asthma, idiopathic pulmonary fibrosis and chronic cough. Spirometry is also helpful in the evaluation of the impact of some systemic diseases on the respiratory system and helps in determining personal risk before surgical intervention.
What do we need to do?
Before the test
When performing spirometry, consider potential contraindications (Table 1). This test is highly dependent on the person’s collaboration and the testing circumstances, therefore, the procedure should be explained beforehand and a decision made by the prescribing physician if the person should stop taking any respiratory medications prior to the test (see Table 2 for minimum timings). It may not be necessary to withhold medication if the purpose of the test is to determine whether the person’s lung function can be improved with therapy in addition to their regular treatment. Instruct the person not to smoke, vape or use a water pipe and abstain from any strenuous physical exercise for at least one hour prior to the test, or to consume intoxicants up to 8 hours before the test. Ask them to loosen any tight clothing. Spirometry must be conducted in a comfortable and well-ventilated room (ideally, specific for spirometry), with the person sitting on a chair without arms, wheels or height adjustment. There must be scales, a stadiometer and a basic weather station (if not already integrated with the test equipment). The spirometer should have a maximum error range of ±2.5% when tested with a 3L calibration syringe.
Table 1: Contraindications for spirometry
Any situation that puts the person's health at serious risk when making a significant effort such as:
- Significant haemoptysis
- Active or recent pneumothorax. Having a pneumothorax in the past does not contraindicate spirometry
- Unstable CV disease (e.g. angina, recent MI, PTE)
- Brain, thoracic or abdominal aneurysms
- Recent retinal detachment or recent eye surgery (e.g. cataracts)
- Recent chest or abdominal surgery
Situations in which minimal acceptable quality manoeuvres cannot be obtained such as:
- Inability to understand directions or unwillingness to follow the directions
- Not understanding the manoeuvre well (e.g. children under 6 years old, mental deterioration, some elderly people)
- Poor physical state (e.g. cachexia)
- Presence of a tracheotomy. If it is considered necessary to perform spirometry on a person with a tracheostomy, they should be referred to a specialist clinic
- Oral and/or facial problems that prevent correct sealing of the mouth around the mouthpiece (e.g. facial paralysis)
- Uncomfortable nausea when inserting the mouthpiece
CV, cardiovascular; MI, myocardial infarction; PTE, pulmonary thromboembolism.
Preparing the person for spirometry
Not all people will be able to produce good quality spirometries, but the operator's competence can improve the quality of the results
- Input the person’s data including age, height and sex at birth into the spirometer.
- Ask them to remove any dental prostheses if they are likely to move.
- Seat them in a chair without arms, wheels or height adjustment with their back against its backrest and both feet flat on the ground, uncrossed. Advise them to sit upright (avoid leaning forward) while blowing.
- Explain the procedure simply: “This is a straightforward test but you will need to follow my instructions closely. When I say ‘inhale deeply and fully’ clasp your teeth on to the mouthpiece, with your lips tightly sealed and your tongue out of the way then blast the air out as fast and hard as you can for as long as you can until your lungs are completely empty or I tell you to breathe in again. Then breathe in deeply and fully again.”
- After explaining, show the patient the procedure by demonstrating a full forced vital capacity (FVC) and forced inspiratory vital capacity (FIVC).
- Adjust the mouthpiece assembly to an appropriate height for the person, ensuring their chin is at a 90o angle to their chest. Ask them to place the mouthpiece between their lips and make sure their tongue does not obstruct the opening.
- If you are testing inspiration, then provide and ask them to wear a tight-fitting nose clip to avoid unnecessary leaks. It is not needed for the expiratory manoeuvre.
- The person must be given a clear and assertive command to initiate the forced breathing. There must be no more than 2 seconds between the end of the inhalation and the start of the forced expiration manoeuvre (hesitation time).
- The flow-volume loop on the screen must be monitored at all times for any alteration that may force the manoeuvre to be stopped.
- The person must be strongly encouraged throughout the whole of the manoeuvre, motivated with exclamations such as: “Go on, go on!” or “Blow out, blow out!”. This step is crucial to ensuring a successful manoeuvre.
- Repeat the test until you have three acceptable and repeatable curves (with a maximum of 8 attempts); more attempts can be considered if the person is feeling well and agrees to further blows.
See Table 3 for the differences in technique for conducting open- or closed-circuit spirometry (which includes a step involving forced breathing).
Table 3: Instructions for people undergoing open-circuit spirometry and closed-circuit spirometry
Open-circuit spirometry
- Sit upright with your legs uncrossed and your feet flat on the floor, without leaning forward
- Exhale completely and empty your lungs
- Breathe in quickly and deeply until your lungs are completely full
- Immediately place the mouthpiece in your mouth and close your lips to form an airtight seal
- Without pausing for >2 seconds, blow out as hard and fast as possible, until your lungs are completely empty or you can’t blow out any more
- Remove the mouthpiece and breathe normally
Closed-circuit spirometry
- Sit upright with your legs uncrossed and your feet flat on the floor, without leaning forward
- Place the mouthpiece in your mouth and close your lips to form an airtight seal
- Breathe normally for 2–3 breaths
- Breathe in quickly and deeply until your lungs are completely full
- Without pausing for >2 seconds, blow out as hard and fast as possible and for as long as possible, until your lungs are completely empty or you can’t blow out any more
- Keeping the mouthpiece tightly sealed against your lips, breathe in again as forcefully and fully as possible
- Remove the mouthpiece and breathe normally
Main variables obtained
Although modern spirometers can yield multiple-variable results, three basic parameters are enough to interpret them: the FVC measured in litres, the forced expiratory volume in the first second (FEV1), a flow measurement expressed in litres per second, and their ratio (FEV1/FVC) given as a ratio or percentage.
- The FVC is the total air volume that can be forcefully exhaled after taking the deepest breath possible. Make sure the person has emptied all the available air from their lungs to finish the manoeuvre.
- The FEV1 is the volume exhaled in the first second of a forced expiratory manoeuvre.
- The relation between the forced exhaled volume in the first second and the forced vital capacity (FEV1/FVC), also known as the forced expiratory ratio (FER or FEV1%), indicates the percentage of the vital capacity exhaled during the first second of the manoeuvre. It is the key parameter for measuring airways obstruction.
Diagnosis of obstructive airway disease
Under normal conditions, in the first second of the forced expiration, over 70% of the FVC is exhaled. If the FEV1/FVC ratio is below 70%, it means that there is an airway obstruction.
To reduce underdiagnosis of obstruction in young patients and overdiagnosis in the elderly, which happens when using the fixed limit of 70%, we propose to use the Lower Limit of Normal (LLN) of the FEV1%, as the cut-off value to determine the presence of an obstruction, which corresponds to the fifth percentile, or to -1.64 on the z-score of the reference value. However the LLN is not included in the software of most current spirometers, and is only indicated without the need for further conversions in the theoretical values of the Global Lung Function Initiative (GLI).(7) For now, 70% remains the cut-off point for obstruction recommended by international organisations, such as the Global Initiative for Chronic Obstructive Lung Disease (GOLD),(8,9) when assessing people with COPD.
Result interpretation
Types of spirometric curves
The first step in the correct interpretation of a spirometry result is to check the acceptability of the curves generated during the manoeuvre using two different graphs: the volume-time graph (V-T) and the flow-volume graph (F-V). Review of the curves on each of these graphs will indicate whether the manoeuvre has been performed correctly and can be considered as acceptable, or if there have been significant errors that require a repetition of the test.
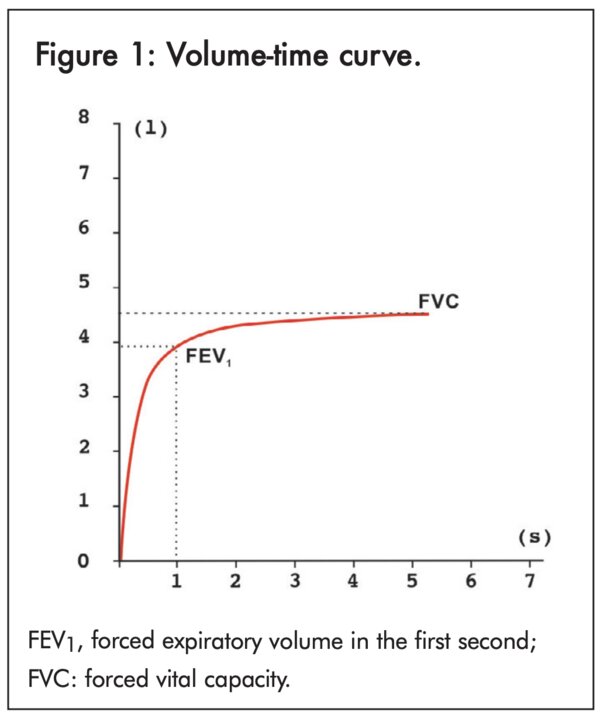
- Volume-time graph: Volume is measured in litres on the y axis (vertical), while time is measured in seconds on the x axis (horizontal). A normal V-T curve has a steep rise, given that a large proportion of the air is expelled in the first second. Following this, the slope becomes gradually smoother until flattening out, when it reaches maximum volume (FVC). The volume of expelled air in the first second is the FEV1 (Figure 1).
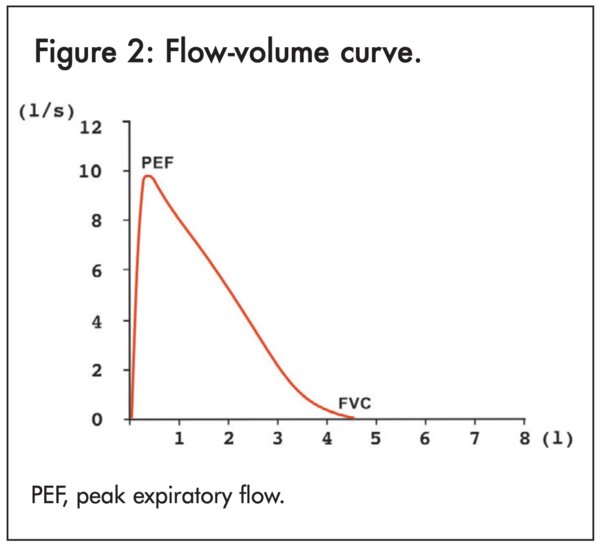
- Flow-volume graph: In this type of graph, flow is measured in litres per second on the y axis (vertical), and the volume is measured in litres on the x axis (horizontal). The normal F-V curve has a very steep rise, near the horizontal axis (flow) until reaching a peak (peak expiratory flow [PEF]). From there, it decreases in a somewhat straight line, with a less pronounced slope, until it finishes by asymptotically reaching the x axis (volume), showing the FVC (Figure 2).
Manoeuvre acceptability
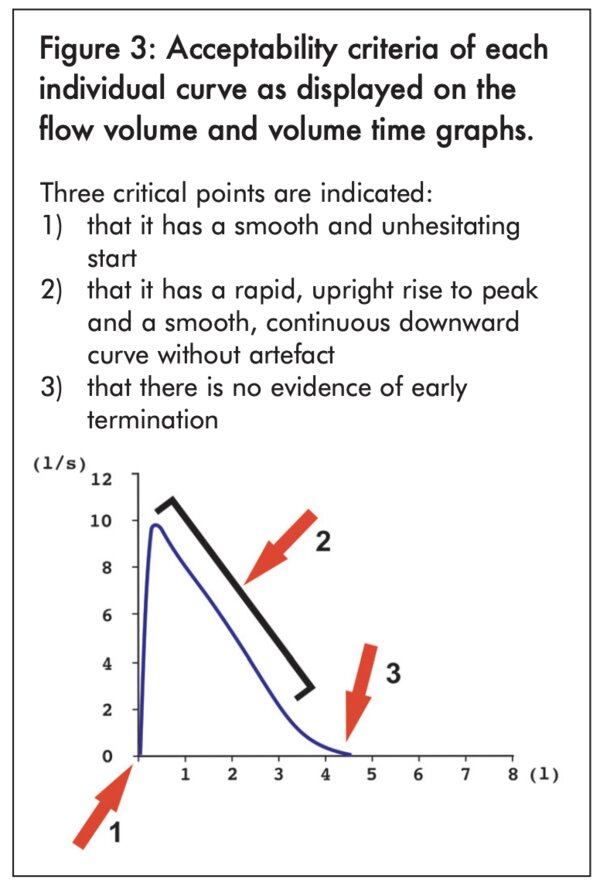
By observing the curves, it is possible to identify a correct manoeuvre and thus meaningful results. The curve must indicate test, and that the peak of effort is very close to the start of the manoeuvre; that the shape of the curve is appropriate, without irregularities pointing at an incorrect or abnormal flow; and that it finishes properly – gradually rather than abruptly – verifying that virtually all of the previously inspired volume was exhaled (Figure 3).
To determine if there has been a good start in each curve, the Back Extrapolated Volume (BEV) (calculated by the spirometer) is used, which must be < 100 ml or 5% of the FVC, whichever is greater.
Manoeuvre repeatability
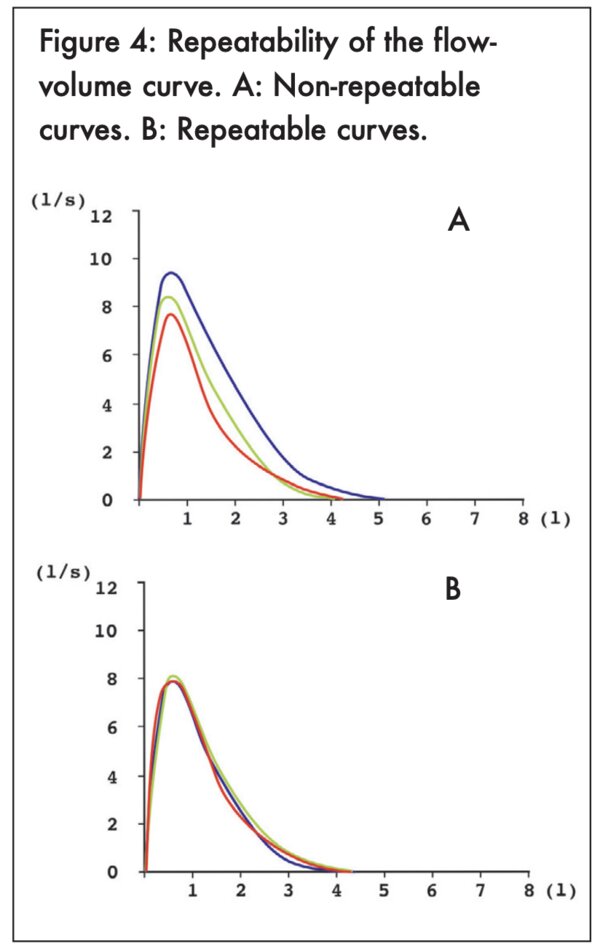
As well as yielding acceptable curves, spirometry must be repeatable in order to be interpreted; we must be sure it will yield similar results every time it is repeated. So, after having obtained at least three acceptable curves, the difference between the two best curves must be less than 150 ml or 5% (for both FVC and FEV1), whichever is greater. In children under 6 years it must be less than 100 ml or 5%, whichever is greater. Most spirometers provide this information automatically (Figure 4).
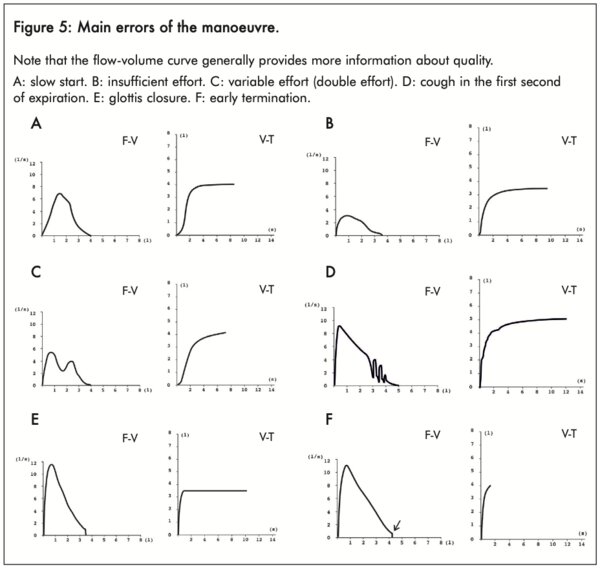
Frequent errors
By observing the curves, it is possible to identify errors by the person and/or operator that may disrupt the test and require a repetition (Figure 5).
- Flow-volume graph: In this type of graph, flow is measured in litres per second on the y axis (vertical), and the volume is measured in litres on the x axis (horizontal). The normal F-V curve has a very steep rise, near the horizontal axis (flow) until reaching a peak (peak expiratory flow [PEF]). From there, it decreases in a somewhat straight line, with a less pronounced slope, until it finishes by asymptotically reaching the x axis (volume), showing the FVC (Figure 2).
Manoeuvre acceptability
By observing the curves, it is possible to identify a correct manoeuvre and thus meaningful results. The curve must indicate test, and that the peak of effort is very close to the start of the manoeuvre; that the shape of the curve is appropriate, without irregularities pointing at an incorrect or abnormal flow; and that it finishes properly – gradually rather than abruptly – verifying that virtually all of the previously inspired volume was exhaled (Figure 3).
To determine if there has been a good start in each curve, the Back Extrapolated Volume (BEV) (calculated by the spirometer) is used, which must be < 100 ml or 5% of the FVC, whichever is greater.
Manoeuvre repeatability
As well as yielding acceptable curves, spirometry must be repeatable in order to be interpreted; we must be sure it will yield similar results every time it is repeated. So, after having obtained at least three acceptable curves, the difference between the two best curves must be less than 150 ml or 5% (for both FVC and FEV1), whichever is greater. In children under 6 years it must be less than 100 ml or 5%, whichever is greater. Most spirometers provide this information automatically (Figure 4).
Most spirometers display warning messages when errors are detected, either on the screen or the hard-copy report. The healthcare professional interpreting the results must take these messages into account. Table 4 shows a summary of the main acceptability and repeatability criteria.
Table 4: Summary of acceptability and repeatability criteria (2)
Acceptability:
Good start:
- Hesitation time <2 seconds
- Back extrapolated volume (BEV) <5% of the FVC or 100 mL, whichever is greater
Good FV curve morphology
- PEF should be achieved with a sharp rise and occur close to Time 0 as measured by the rise time from 10% to 90% of peak flow, which should be <150 ms
- Smooth, continuous downward curve: no cough, no obstruction, no leak, no glottis closure (early termination), no extra breaths
Smooth completion of the manoeuvre
Must meet at least one of the following criteria:
- Achieved an expiratory plateau (≤25 mL in the last 1 second of expiration)
- Achieved an expiratory time ≥15 seconds
- FVC is within the repeatability tolerance of, or is greater than, the largest prior observed FVC Forced. If the maximal inspiration after end of force exhalation is greater than FVC, then FIVC must be <5% of FVC or 100 ml, whichever is greater.
Repeatability
The difference in values between the two best curves (of at least 3 performed that meet the acceptability criteria) must be less than 150 ml, both for FVC and FEV1
FET, forced expiration time; FEV1, forced expiratory volume in the first second; FV, flow-volume; FVC, forced vital capacity; PEF, peak expiratory flow; VT, volume-time.
Spirometry results
Reference values
The results obtained from the spirometry test must be interpreted against reference or theoretical values for healthy people of the same age, height and sex at birth. The values obtained for each person are compared with these predicted values and are expressed as a percentage of the observed value in relation to the theoretical value (observed value/ theoretical value x 100). A 100% value means that the observed parameter equals the theoretical. Regarding the FVC and the FEV1, a value ≥80% of the theoretical value is considered normal, while a value <80% is considered pathological. Similar to the explanation about the FEV1%, it would be advisable to use the LLN rather than the fixed value of 80% of the theoretical value in order to avoid over- or underestimating the results in some of the cases.
Utilising the reference values by the GLI-2012 is recommended.
Spirometric patterns
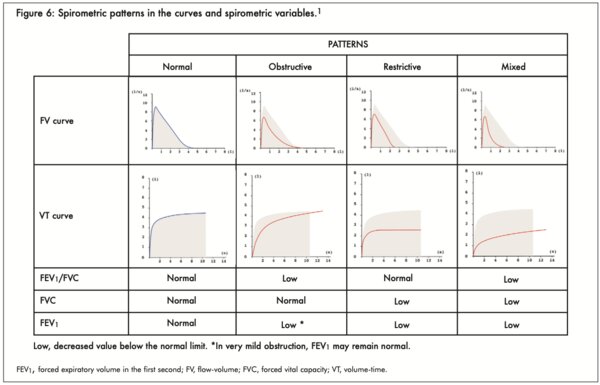
The interpretation of an acceptable and repeatable manoeuvre is reasonably straight-forward, given that only 4 different, easily distinguishable spirometric patterns are possible.
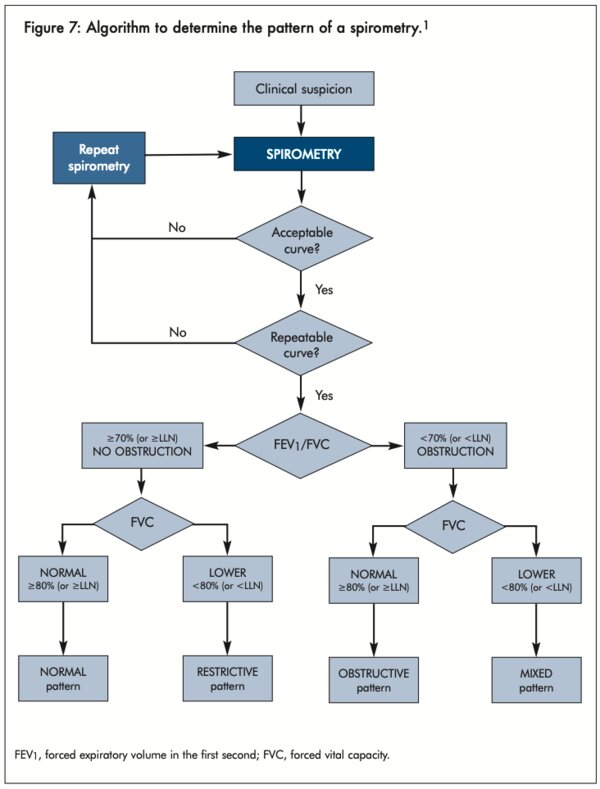
A simple observation of the curves can reveal the test pattern, although it is advisable to verify them through the evaluation of the numerical values (Figure 6). To define the spirometric patterns, apply the algorithm in Figure 7.
Result application in clinical practice
Spirometry does not provide a diagnosis in and of itself - it merely supports or contradicts a suspected diagnosis, based on related clinical data and other complementary tests. However, spirometry does provide valuable clues, and by analysing its results, it is possible to identify four spirometric patterns: normal, obstructive, restrictive and mixed. These distinct patterns, together with the person's clinical data, make it possible to make a diagnosis.
Post-bronchodilator responsiveness test
The Bronchodilator (BD) Responsiveness Test is used to study the dilation that can occur in the person's bronchi after being administered a bronchodilator (usually salbutamol/ albuterol), and whether that bronchodilation reaches full reversibility (normalisation of a previously obstructive pattern). FVC pre- and post-BD are compared. If there is >10% of predicted value improvement in either the FEV1 or FVC the test is considered to have a positive BD response. The previous criteria for a positive BD test of >200 ml has been recently removed from ERS-ATS guidelines to simplify the interpretation of the test.
Next steps
In cases where spirometry reveals a mixed pattern (obstruction + restriction), the person should be referred for a lung volume test (e.g., plethysmography), to evaluate whether the reduced FVC is due to restrictive disease, or is just a functional restriction of the volume due to air trapping, with an increase in the residual volume, which happens to the vast majority of people with severe cases of COPD.
References
- Cimas Hernando JE, Calvo Corbella E, Perez Fernandez J, et al. Guía de procedimiento para la espirometría en atención primaria. Barcelona: semFYC ed, 2021.
- Graham BL, Steenbruggen I, Miller MR, et al. Standardization of Spirometry 2019 Update. An official American Thoracic Society and European Respiratory Society Technical Statement. Am J Respir Crit Care 2019; 200:e70–e88.
- Miller MR,Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J 2005;26:319–38.
- National Asthma Council Australia. The spirometry handbook for primary care. Melbourne; National Asthma Council Australia: 2020. Available at: https://www.nationalasthma.org.au/living-with-asthma/resources/health-professionals/information-paper/spirometry-handbook Accessed March 2023.
- García-Río F, Calle M, Burgos F, et al. Spirometry. Spanish Society of Pulmonology and Thoracic Surgery (SEPAR). Arch Bronconeumol 2013;49: 388–401.
- Global Initiative for Asthma (GINA). Global Strategy for Asthma Management and Prevention, Updated 2021. Available at: https://ginasthma.org/wp-content/uploads/2021/05/GINA-Main-Report-2021-V2-WMS.pdf Accessed March 2023.
- Quanjer PH, Stanojevic S, Stocks J, Cole TJ. GLI-2012. All-age multi-ethnic reference values for spirometry. Available at: https://www.ers-education.org/lrmedia/2012/pdf/266696.pdf. Accessed March 2023.
- Global Initiative for Chronic Obstructive Lung Disease: 2022 Report. Available at: https://goldcopd.org/2022-gold-reports-2/. Accessed March 2023.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Spirometry guide: Spirometry for health care providers. Available at: https://goldcopd.org/gold-spirometry-guide/. Accessed March 2023.
- Stanojevic S, Kaminsky DA, Miller MR, et al. ERS/ATS technical standard o interpretive strategies for routine lung function tests. Eur Respir J 2022;60: 2101499.
Additional information
- Authors: Miguel Roman Rodriguez, Juan Enrique Cimas
- Reviewers: Lindsay Zurba, Savi Wimalasekera, Sundeep Salvi, Siân Williams
- Editor: Patima Tanapat (Integrity Continuing Education, Inc) and Tracey Lonergan (IPCRG)
Additional administrative support was provided by Stefani Chiarolanza and Samuel Ciociola (Integrity Continuing Education, Inc) and Russel Emeny (IPCRG). This desktop helper is advisory; it is intended for general use and should not be regarded as applicable to a specific case. More information is available at: www.ipcrg.org/DTH14.
Creative Commons Licence Attribution-NonCommercial-ShareAlike
The IPCRG is a registered charity [SC No 035056) and a company limited by guarantee (Company No 256268). Communication address: 19 Armour Mews, Larbert, FK5 4FF, Scotland, United Kingdom.
Resource information
- Asthma
- Chronic Breathlessness
- COPD
- Diagnosis
- Disease management
- Spirometry
- Asthma Right Care
- COPD Right Care
- Asthma
- COPD
- Diagnosis
- Management
- Clinical Education