Desktop Helper No. 20 - A practical guide to improve rhinitis management in primary care - online version
This is an online version of Desktop Helper No. 20 - A practical guide to improve rhinitis management in primary care. Visit the linked page for a PDF, translations, more information and related resources. References are available at the bottom of the page.
Allergic rhinitis (AR) is a common condition affecting between 15-25% of the general population; its symptoms significantly reduce quality of life and pose a high economic burden, including indirect costs related to lost school and workdays.(1,2) Studies of people consulting general practitioners for AR found that 18–48% had symptoms uncontrolled by pharmacotherapy.(3-5) Despite the bothersome nature of symptoms, AR is often trivialised by those with AR – only 45% seek medical advice or treatment, which results in under-treatment and poor symptom control.(6) AR is strongly associated with an increased risk of developing asthma – approximately 20–30% of people with AR also have asthma.(7,8) These persons tend to be sensitised to multiple allergens.(9) Anybody with confirmed AR should be screened for asthma. Those with AR are more likely to have frequent asthma exacerbations and poorer symptom control than those with only asthma.(6) People with both asthma and AR also frequently have more persistent and severe AR symptoms and therefore experience a greater loss of school and work productivity.(10-12)
Introduction
Accurate diagnosis of rhinitis is crucial as underdiagnosis and misclassification lead to ineffective treatment, unnecessary costs and impaired quality of life (see Desktop Helper No.19). Rhinitis is broadly classified into allergic (AR): IgE-mediated, triggered by allergens such as pollen/dust mites; non-allergic (NAR): not triggered by allergens, e.g., vasomotor, drug-induced, or infectious; and mixed phenotypes.(13) The Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines emphasise the unified airway link between AR and asthma, advocating for:
- Phenotype-driven management (intermittent or persistent; mild or moderate-severe)
- Combined pharmacotherapy (for moderate- severe cases)
- Allergen immunotherapy for refractory cases
This desktop helper translates these principles into actionable steps for primary care.
Perceptions and concerns of persons with rhinitis
- An under-recognised condition: rhinitis – whether AR or NAR – is often viewed as an everyday part of life. People generally see nasal symptoms like sneezing, congestion, a runny nose, and itching as temporary and harmless, often linked to weather changes, dietary triggers, or dust exposure. Rhinitis is frequently accompanied by disregarded ocular symptoms such as itching, tearing (or lacrimation) and injected conjunctivae (bloodshot eyes). AR is often mistaken for a common cold that does not go away, or as a “summer” cold, especially during seasonal changes. NAR, such as irritant-induced symptoms from pollution or strong odours, is often viewed as unavoidable. Infectious rhinitis, typically viral, is commonly self-treated with over-the-counter medications without seeking care. Although increasingly relevant in urban and industrial settings, occupational rhinitis is rarely recognised or linked to workplace exposure.
- People with rhinitis tend to seek rapid symptom relief, often resorting to OTC self-medication and stop treatment once they feel better. They don’t necessarily expect a structured diagnosis or management plan and only tend to seek help when symptoms are no longer tolerable.14 Therefore a considered diagnosis, preventive care, allergen identification, and long-term medication use are uncommon. However, many express concerns about the side effects of corticosteroid nasal sprays, which, when used properly are negligible, whereas topical nasal decongestants may cause dependence. A Visual Analogue Scale (VAS) of 0 (no symptoms) to 10 (very severe symptoms) is the simplest validated way to assess symptoms and the impact of treatment (see Desktop Helper No.19).
- Overlooked links between rhinitis, asthma, and sinusitis: There is limited awareness of the chronic nature of certain types of rhinitis and their effects on daily life, sleep, productivity (absenteeism and presenteeism), and mental health. Additionally, the potential overlap of rhinitis or chronic rhinosinusitis with asthma or COPD is often overlooked, leading to missed opportunities for early intervention: NSAID exacerbated respiratory disease (N-ERD) is such an example.(15)
- Reframing rhinitis as a manageable condition: addressing these perceptions requires targeted education. Healthcare providers should explain the different forms of rhinitis, their underlying causes, and the importance of appropriate care according to the underlying type of rhinitis. Just as public awareness of oral health has improved over time, a similar shift is needed for nasal health: moving public belief from rhinitis being considered as an unavoidable “nuisance” to a “manageable condition” is essential for improving outcomes.
Rhinitis is not trivial, harmless, or unmanageable. Primary care clinicians can support people suffering from rhinitis by helping them understand that attention to triggers, symptoms, and effective treatment can significantly reduce discomfort and improve quality of life.
Patient education and self-management - see BOX 1
Box 1 Patient education and self-management
Consider discussing with persons struggling with rhinitis:
Rhinitis is a common condition that affects the nose (and frequently the eyes) and can make daily life uncomfortable. Learning about it and how to manage it can help you feel better and live more comfortably.
What does the nose do?
Your nose is not just for smelling! It works as a gatekeeper and air conditioner for your lungs. It:
- Filters out dust and particulate matter
- Warms the air you breathe in
- Adds moisture so the air is not too dry.
When your nose is not working correctly, it can affect your breathing and overall health.
What is rhinitis?
Rhinitis means inflammation (swelling) inside the nose, affecting how your nose works. Common symptoms include:
- Sneezing
- Itchy nose
- Stuffy nose (nasal congestion)
- Runny nose or postnasal drip (a sensation of mucus at the back of the throat, causing you to clear your throat)
- Itchy eyes (present in at least 50% of the patients with AR).
Types of rhinitis
- Allergic rhinitis: triggered by pollens, dust mites, pet dander, moulds, etc.
- Non-allergic rhinitis: caused by irritants such as smoke, strong smells, cold air, or spicy food
- Infectious rhinitis: usually from viruses like the common cold
- Occupational rhinitis: caused by exposures at work, such as exposure to chemicals or dust.
How can you prevent rhinitis?
- If possible, avoid your triggers (like dust, pollen, smoke, etc.)
- Keep your nose clean: practise good nasal hygiene (see below)
- Take the correct medications for your type of rhinitis
- Learn how to manage your symptoms at home
- Ensure good indoor air quality, if possible.
Self-management tips: how to take control of your rhinitis
- Know and follow your treatment plan
- Take medications as prescribed
- Keep a diary of your moderate to severe symptoms, as this can also help you identify your triggers
- Clean your nose regularly (see below)
- Do not overuse decongestants (in nasal sprays or drops), which should not be used for more than 5 continuous days
- Go back to your doctor if things do not improve or change
Nasal hygiene is a key preventive measure. Just as brushing teeth (oral hygiene) prevents gum disease, regular nasal cleaning helps prevent rhinitis.
Daily nasal hygiene checklist
- Rinse your nose daily, gently, with normal saline; during exacerbations, you can also use a nasal douching or a squirt bottle (after being shown how).
- Clean your nose after exposure to dust or smoke.
Make it a habit, just like brushing your teeth!
Sinus Rinse Animation (36’’)
How to Wash your Nose (4’56’’)
When should I see a doctor?
- Your nasal and/or eye symptoms last more than 2–4 weeks
- Medications are not helping
- You also have asthma that is getting worse
- Your sleep or daily activities are affected
- You are not sure what is causing your symptoms
- You have 2 or more of: nasal blockage and/or discharge, fever, facial pain, partial loss of smell lasting more than 10 days, or, importantly, deteriorating after 5 days.
- You are having trouble breathing (other than that caused by a blocked nose).
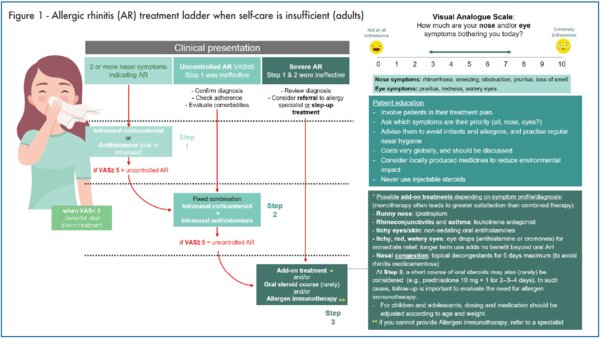
Management of rhinitis where self-care is insufficient (see Figure 1)
Allergic rhinitis
In the majority of the cases, people with AR symptoms self-manage and stop treatment once they feel better (particularly in mild intermittent AR), without consulting a primary care clinician.(14) However, it is important to identify those with uncontrolled rhinitis who require further care. Pharmacists could play a key role in recognising such patients and referring those with moderate/severe symptoms to primary care. Once identified, and after evaluating the person’s symptoms, commence baseline treatment (see Figure 1). Reassess after 14 days and discuss with the person (or the caregiver) whether the treatment plan needs adjusting.
Medications for the treatment of rhinitis are listed in Annex 1. They may be available as OTC or by prescription only, depending on local regulations and availability. Not all medicines are accessible in every country.
The pharmacotherapy should be adapted to the severity and frequency of symptoms:
- As-needed therapy may be sufficient for patients with mild intermittent symptoms, including those with predictable allergen exposure (e.g. pets).
- Daily therapy is most effective for intermittent bouts that typically last about 2 weeks
Intranasal corticosteroids (INCS) have been shown to be more effective than antihistamines (oral and intranasal) for most symptoms.(16) INCS demonstrate incremental benefit over successive days. The onset of action of topical intranasal antihistamines (INAH) is more rapid than oral antihistamines (OAH). In patients with moderate/severe rhinitis, a combined formulation (e.g., azelastine-fluticasone, olapatadine-mometasone) is the preferred treatment for both speed of onset of action and greater efficacy.(16)
Oral leukotriene receptor antagonists (LTRA) are not advised as initial treatment for allergic rhinitis in adults or children, as they are less effective than INCS, INAH, and/ or OAH, and due to safety concerns, particularly neuropsychiatric side effects.17 Their use should only be considered in patients with asthma, or if other therapies fail, or if the patient strongly prefers oral medication, especially when asthma is present.
The use of intranasal cromones is not recommended for nasal symptoms but may be used for ocular symptoms if no other treatment is successful.
Correct administration technique is key for all topical treatments.
How to use a nasal spray (2’26’’)
Teaching patients to use nasal sprays (2’58’’)
Local allergic rhinitis (LAR) is a nasal allergy condition where allergy symptoms are present but all specific IgE determinations or skin prick tests are negative and should be treated preferentially with nasal sprays, but oral antihistamines and allergen immunotherapy (AIT) have also proven to be effective (Annex 1).(18)
Non-allergic rhinitis
One of the key parts of treatment is avoiding identified triggers, which may include tobacco smoke, certain medications, or dietary components (see Desktop Helper No.19).(19) Some factors, such as a runny nose in cold or windy weather, are often unavoidable and usually cause only short-lived symptoms that do not require treatment.
Non-allergic rhinitis especially due to viral infections, can be temporarily treated (for a maximum of 5 continuous days) with decongestant nasal sprays (phenylephrine, oxymetazoline, xylometazoline, naphazoline) but are NOT recommended for regular treatment of allergic rhinitis. Longer use (>5 days) can cause rhinitis medicamentosa!(20)
Not all persons with rhinitis have asthma, but approximately 80% of those with asthma have rhinitis; the more severe the rhinitis, the greater the impact on asthma control and exacerbations.(21-23)
Providing education to persons with rhinitis on how regular/daily use of medication allows maximal benefit to be achieved is important. However, similar to asthma, rhinitis is a variable disease so reducing medication when control is achieved seems a logical step and aligns with the maintenance and reliever therapy (MART) approach for asthma of varying medication according to symptoms. If patients or caregivers ask for guidance on environmentally friendly treatment options, and there is no direct evidence available, the most appropriate option is to recommend a locally produced product to minimise the environmental impact of transportation.(24)
Non-pharmacological treatment of AR, NAR, and Mixed Rhinitis
- Saline irrigation: Nasal irrigation thins and removes mucus, clears proteins that induce inflammation, and flushes out irritants and bacteria from the nasal and sinus cavities. Nasal saline irrigation can be used for persons with AR, NAR, or mixed rhinitis, and is a crucial component of treatment for individuals with chronic rhinosinusitis. In patients with AR, saline irrigation reduces patient-reported disease severity compared with no irrigation.(25-27)
- Other non-pharmacological approaches: environmental measures for managing rhinitis symptoms primarily aim to reduce exposure to allergens and irritants.
- Car filters efficiently trap airborne particles, including pollen, enhancing air quality inside vehicles.(28)
- Sunglasses protect the eyes from allergens, helping to reduce symptoms such as itching and tearing.(28)
- Air purifiers equipped with HEPA filters remove allergens from indoor air, creating a cleaner living environment.(28)
- Well-fitting masks, particularly those designed to filter allergens, help reduce pollen and irritant particles / dust inhalation when outdoors.(28)
- Pollen screens installed on windows and doors serve as fine mesh barriers that prevent allergens from entering homes and workplaces, while still allowing air circulation.
- Pollen forecasts provide valuable information on expected allergen levels, enabling individuals to plan activities and adopt preventive measures accordingly.
These cost-effective environmental interventions decrease allergen exposure and alleviate rhinitis symptoms.(29) By combining these strategies, individuals create a more allergen-controlled environment in their homes, vehicles, and outdoor settings, potentially reducing reliance on pharmacological treatments.29
Role of pharamcists and nurses
Nurses and community pharmacists are uniquely positioned to support people living with rhinitis and improve their quality of life by educating them on symptom management, advising on medication use, and promoting strategies to reduce allergen exposure. Through structured assessments and tailored advice, they help these persons distinguish between AR and NAR, manage their symptoms effectively, and recognise warning signs that require referral. Nurse/community pharmacist communication with GPs and specialists helps ensure continuity of care, while their role in empowering those with rhinitis supports self-management and reduces unnecessary healthcare visits.
Pharmacist-led interventions enhance adherence and clinical outcomes. Pharmacists can ensure the correct use of intranasal inhalers/sprays, which is key to achieving therapeutic efficacy and symptom relief, and support patients to manage their condition more effectively. This role becomes even more important in the context of switching from prescription to over-the-counter (OTC) therapies, where pharmacist-led guidance is likely to be the only professional support persons with rhinitis receive. Viral acute rhinosinusitis, in particular, can often be effectively managed at the pharmacy level through symptom relief and the promotion of self-care.(30-33)
Review: Monitoring and follow-up
How often should persons with rhinitis be reviewed?
In essence, this should depend on response. Full response suggests no need to review, partial response suggests review of adherence, technique,34 and address any non-allergic factors such as smoking or occupational aspects.(35) Non-response, especially when adherence and technique are good, suggests the need for diagnostic review and/or referral. Increasingly, digital tools are likely to have a role in assisting both the patient and clinician to optimise outcomes.(36,37) The MASK-Air app is well established. The use of a structured review improves outcomes,(38,39) as does shared decision-making.(40)
What should be reviewed?
Disease severity, as measured by the rhinitis VAS, treatment adherence and technique, the search for other factors such as NAR, change in occupation, or environmental exposure, and the shared decision-making plan.
When to consider allergen immunotherapy?
Consider allergen immunotherapy (AIT), including sublingual immunotherapy (SLIT), for people with moderate to severe AR whose symptoms remain uncontrolled despite optimal pharmacological therapy. This includes regular use of INCS and INAH, OAH, and appropriate ocular treatments. Strong indications for AIT include symptoms that significantly impair daily functioning, sleep quality, school or work performance, or that persist even with low to moderate allergen exposure. A VAS score of 5 or higher typically indicates inadequate symptom control. A confirmed diagnosis of IgE-mediated allergy is essential, based on clinical history and supported by positive skin-prick testing or specific IgE to relevant allergens.
Access to AIT varies from country to country depending on the organisational model of health care and available resources.
References
- Savouré M, Bousquet J, Jaakkola JJK, Jaakkola MS, Jacquemin B, Nadif R. Worldwide prevalence of rhinitis in adults: A review of definitions and temporal evolution. Clin Transl Allergy. 2022;12(3):e12130
- Bousquet J, Khaltaev N, Cruz AA, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy. Apr 2008;63 Suppl 86:8-160. doi:ALL1620 [pii] 10.1111/j.1398-9995.2007.01620.x
- Bousquet J, Anto JM, Bachert C, et al. Allergic rhinitis. Nat Rev Dis Primers. Dec 3 2020;6(1):95. doi:10.1038/s41572-020-00227-0 (abstract)
- Bhattacharyya N. Incremental healthcare utilization and expenditures for allergic rhinitis in the United States. Laryngoscope. 2011;121(9):1830-3. (abstract)
- Vandenplas O, Vinnikov D, Blanc PD, Agache I, Bachert C, Bewick M, et al. Impact of Rhinitis on Work Productivity: A Systematic Review. J Allergy Clin Immunol Pract. 2018;6(4):1274-86.e9
- Linneberg, A., Dam Petersen, K., Hahn-Pedersen, J., Hammerby, E., Serup-Hansen, N., & Boxall, N. (2016). Burden of allergic respiratory disease: a systematic review. Clinical and molecular allergy: CMA, 14, 12. https://doi.org/10.1186/s12948-016-0049-9
- Tohidinik HR, Mallah N, Takkouche B. History of allergic rhinitis and risk of asthma; a systematic review and meta-analysis. World Allergy Organ J. Oct 2019;12(10):100069. doi:10.1016/j.waojou.2019.100069
- Leynaert B, Neukirch C, Kony S, et al. Association between asthma and rhinitis according to atopic sensitization in a population-based study. J Allergy Clin Immunol. Jan 2004;113(1):86-93.
- Bousquet J, Melen E, Haahtela T, et al. Rhinitis associated with asthma is distinct from rhinitis alone: The ARIA-MeDALL hypothesis. Allergy. May 2023;78(5):1169-1203. doi:10.1111/all.15679
- Scelo G, Torres-Duque CA, Maspero J, et al. Analysis of comorbidities and multimorbidity in adult patients in the International Severe Asthma Registry. Ann Allergy Asthma Immunol. Jan 2024;132(1):42-53. doi:10.1016/j.anai.2023.08.021
- Halpern MT, Schmier JK, Richner R, Guo C, Togias A. Allergic rhinitis: a potential cause of increased asthma medication use, costs, and morbidity. J Asthma. Feb 2004;41(1):117-26.
- Clatworthy J, Price D, Ryan D, Haughney J, Horne R. The value of self-report assessment of adherence, rhinitis and smoking in relation to asthma control. Prim Care Respir J. 2009 Dec;18(4):300-5.
- Bousquet J, Schünemann HJ, Togias A, Bachert C, Erhola M, Hellings PW, Klimek L, Pfaar O, Wallace D, Ansotegui I, Agache I. Next-generation Allergic Rhinitis and Its Impact on Asthma (ARIA) guidelines for allergic rhinitis based on Grading of Recommendations Assessment, Development and Evaluation (GRADE) and real-world evidence. Journal of Allergy and Clinical Immunology. 2020 Jan 1;145(1):70-80.
- Bousquet J, Neukirch F, Bousquet PJ, Gehano P, Klossek JM, Le Ga M et al. Severity and impairment of allergic rhinitis in patients consulting in primary care. J Allergy Clin Immunol 2006;117:158–162.
- Romano A, et al. "Updating the classification and routine diagnosis of NSAID hypersensitivity reactions: A WAO Statement." World Allergy Org J 18.8 (2025): 101086.
- Sousa-Pinto B, Vieira RJ, Brozek J, Cardoso-Fernandes A, Lourenço-Silva N, Ferreira-da-Silva R, Ferreira A, Gil-Mata S, Bedbrook A, Klimek L, Fonseca JA, Zuberbier T, Schünemann HJ, Bousquet J. Intranasal antihistamines and corticosteroids in allergic rhinitis: A systematic review and meta-analysis. J Allergy Clin Immunol. 2024 Aug;154(2):340-354.
- Lo CW, Pathadka S, Qin SX, Fung LW, Yan VK, Yiu HH, Bloom CI, Wong IC, Chan EW. Neuropsychiatric events associated with montelukast in patients with asthma: a systematic review. European Respiratory Review. 2023 Sep 27;32(169).
- Campo P, Eguiluz‐Gracia I, Bogas G, Salas M, Plaza Serón C, Pérez N, Mayorga C, Torres MJ, Shamji MH, Rondon C. Local allergic rhinitis: implications for management. Clinical & Experimental Allergy. 2019 Jan;49(1):6-16.
- Hellings PW, Klimek L, Cingi C, et al. Non-allergic rhinitis: position paper of the European Academy of Allergy and Clinical Immunology. Allergy. 2017;72(11):1657–65. doi:10.1111/all.13200.
- Li LJ, Wang SY, Tsai CY, Wu CJ. Rhinitis medicamentosa. BMJ Case Rep. 2021 Nov 9;14(11):e247051. doi: 10.1136/bcr-2021-247051. PMID: 34753736; PMCID: PMC8578967.
- Clatworthy J, Price D, Ryan D, Haughney J, Horne R. The value of self-report assessment of adherence, rhinitis and smoking in relation to asthma control. Primary Care Respiratory Journal. 2009 Dec;18(4):300-5.). Managing the rhinitis with INS or INS?INAH combinations improves asthma control and QoL
- Scichilone, N. et al. The effect of intranasal corticosteroids on asthma control and quality of life in allergic rhinitis with mild asthma. J. Asthma 48, 41–47 (2011)
- De Jong HJ, Voorham J, Scadding GK, Bachert C, Canonica GW, Smith P, Wahn U, Ryan D, Castillo JA, Carter VA, Murray RB. Evaluating the real-life effect of MP-AzeFlu on asthma outcomes in patients with allergic rhinitis and asthma in UK primary care. World Allergy Organization Journal. 2020 Dec 1;13(12):100490
- Vieira RJ, Sousa-Pinto B, Herrmann A, Antó J Williams S, Bognanni A, Pereira AM, Haahtela T, Leontiadis GI, Pfaar O, Valiulis A, Zuberbier T, Piggott T, Schünemann HJ, Bousquet J; ARIA 2024-2025 Guideline Panel. A Novel Approach to Consider Planetary Health in Guideline Development: A GRADE Approach Using the Allergic Rhinitis and its Impact on Asthma (ARIA) 2024-2025 Guidelines as a Case Study. J Allergy Clin Immunol Pract. 2025 Jun 10:S2213-2198(25)00538-0. doi: 10.1016/j.jaip.2025.04.060. Epub ahead of print. PMID: 40505857.
- Fokkens WJ, Lund VJ, Hopkins C, Hellings PW, Kern R, Reitsma S et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2020. Rhinology. 2020 Feb 20;58(Suppl S29):1-464. doi: 10.4193/Rhin20.600. PMID: 32077450.
- Head K, Snidvongs K, Glew S, Scadding G, Schilder AG, Philpott C, Hopkins C. Saline irrigation for allergic rhinitis. Cochrane Database Syst Rev. 2018 Jun 22;6(6):CD012597. doi: 10.1002/14651858.CD012597.pub2. PMID: 29932206; PMCID: PMC6513421.
- Hermelingmeier KE, Weber RK, Hellmich M, Heubach CP, Mösges R. Am J Rhinol Allergy. 2012 Sep-Oct;26(5):e119-25. doi: 10.2500/ajra.2012.26.3787.Nasal irrigation as an adjunctive treatment in allergic rhinitis: a systematic review and meta-analysis.
- Schutzmeier P, Kutzora S, Mittermeier I, Becker J, Bergmann KC, Böse-O'Reilly S, Buters J, Damialis A, Heinrich J, Kabesch M, Mertes H, Nowak D, Korbely C, Walser-Reichenbach S, Weinberger A, Heinze S, Steckling-Muschack N, Herr C. Non-pharmacological interventions for pollen-induced allergic symptoms: Systematic literature review. Pediatr Allergy Immunol. 2022 Jan;33(1):e13690.
- Bergmann KC, Berger M, Klimek L, Pfaar O, Werchan B, Werchan M, Zuberbier T. Nonpharmacological measures to prevent allergic symptoms in pollen allergy: A critical review. Allergologie Select. 2021;5:349.
- Blaiss MS, Steven GC, Bender B, Bukstein DA, Meltzer EO, Winders T. Shared decision making for the allergist. Ann Allergy Asthma Immunol. 2019 May;122(5):463-470. doi: 10.1016/j.anai.2018.08.019. Epub 2018 Sep 7. PMID: 30201469.
- Scheire S, Germonpré S, Mehuys E, Van Tongelen I, De Sutter A, Steurbaut S, Van Hees T, Demarche S, Lahousse L, Gevaert P, Boussery K. Rhinitis Control and Medication Use in a Real-World Sample of Patients With Persistent Rhinitis or Rhinosinusitis: A Community Pharmacy Study. J Allergy Clin Immunol Pract. 2024 Jul;12(7):1865-1876.e6. doi: 10.1016/j.jaip.2024.04.031. Epub 2024 Apr 25. PMID: 38677586.
- House R, Kritikos V, Cvetkovski B, Rimmer J, Yan K, Cheong L, Bousquet J, Lourenco O, Bosnic-Anticevich S. The impact of implementing an allergic rhinitis clinical management pathway (AR-CMaP) in the community pharmacy. Explor Res Clin Soc Pharm. 2023 Oct 5;12:100340. doi: 10.1016/j.rcsop.2023.100340. PMID: 37869069; PMCID: PMC10585337.
- Lourenço O, Cvetkovski B, Kritikos V, House R, Scheire S, Costa EM, Fonseca JA, Menditto E, Bedbrook A, Bialek S, Briedis V, Boussery K, Canonica GW, Haahtela T, Kuna P, Mullol J, Orlando V, Samolinski B, Wallace D, Duggan C, Paulino E, Pinto GS, Söderlund LÅ, Bousquet J, Bosnic-Anticevich S. Management of allergic rhinitis symptoms in the pharmacy Pocket guide 2022. Clin Transl Allergy. 2022 Oct 5;12(10):e12183. doi: 10.1002/clt2.12183. PMID: 36225265; PMCID: PMC9533218.
- Rollema C, van Roon EN, de Vries TW. Inadequate quality of administration of intranasal corticosteroid sprays. Journal of asthma and allergy. 2019 Apr 3:91-4.
- Mungan D. Occupational allergic rhinitis: what do we know?. Current Treatment Options in Allergy. 2015 Mar;2:10-9.
- Zhang H, Cao Y, Jiang H, Zhou Q, Yang Q, Cheng L. The present and future of digital health, digital medicine, and digital therapeutics for allergic diseases. Clinical and translational allergy. 2025 Jan;15(1):e70020
- Matricardi PM, Dramburg S. Digital allergology: from theory to practice. Springer Nature; 2025 Apr 21.
- Scheire S, Germonpré S, Mehuys E, Van Tongelen I, De Sutter A, Steurbaut S, Van Hees T, Demarche S, Lahousse L, Gevaert P, Boussery K. Rhinitis control and medication use in a real-world sample of patients with persistent rhinitis or rhinosinusitis: a community pharmacy study. The Journal of Allergy and Clinical Immunology: In Practice. 2024 Jul 1;12(7):1865-76
- Price DB, Scadding G, Bachert C, Saleh H, Nasser S, Carter V, Von Ziegenweidt J, Durieux A, Ryan D. UK prescribing practices as proxy markers of unmet need in allergic rhinitis: a retrospective observational study. NPJ primary care respiratory medicine. 2016 Jun 23;26(1):1-8
- Steven GC. Shared decision making in allergic rhinitis: an approach to the patient. Annals of Allergy, Asthma & Immunology. 2020 Sep 1;125(3):268-72
- Scadding GK, Conti DM, Scheire S, Backer V, et al EUFOREA meeting on defining disease states in allergic rhinitis: towards a unified language in AR. Frontiers Allergy. 2025 Feb 3;5:1531788.
Additional information
Authors: Dermot Ryan, Jaime Correia de Sousa, Olga Lourenço, Björn Stridh, Stephanie Dramburg, Monsur Habib, Sarah Ben Hamida, Luís Carvalho, Siân Williams
Reviewers: Mário Morais-Almeida, Jean Bousquet
Editor: Ian Wright
Funding statement: This desktop helper was funded from an educational grant from ALK-Abelló who provided a grant to support the development, typesetting, printing and associated costs but did not contribute to the concept or content of this document.
This desktop helper is advisory; it is intended for general use and should not be regarded as applicable to a specific case.
Creative Commons Licence Attribution-NonCommercial-NoDerivatives.
The IPCRG is a Scottish-registered charity (No. 035056) and a Scottish company limited by guarantee (Company No. SC256268). Communication address: 19 Armour Mews, Larbert, FK5 4FF, Scotland, United Kingdom.
Resource information
- Allergic rhinitis
- Rhinitis
- Disease management
- Rhinitis Right Care